You just had your annual screening mammogram and the summary report provided to you states you have “dense” breasts but this is a BENIGN FINDING and there is no evidence of breast cancer. The language used in the report may be mandated by law, and say something like, “Your mammogram shows that your breast tissue is dense. Dense breast tissue is common and is not abnormal. However, dense breast tissue can make it harder to evaluate the results of your mammogram and may also be associated with an increased risk of breast cancer. This information about the results of your mammogram is given to you to raise your awareness and to inform your conversations with your doctor. Together, you can decide which screening options are right for you. A report of your results was sent to your physician.”
What Are Dense Breasts?
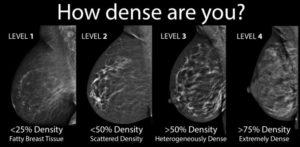
Breast density describes the amount of glandular tissue in the breast, meaning dense breasts have less fatty tissue than normal breasts. Here is the classification system used by radiologists interpreting your mammogram:
Why Are Dense Breasts Concerning?
High breast density, as seen on a mammogram, is linked to an increased risk of breast cancer. Women with very dense breasts are four to five times more likely to develop breast cancer than women with low breast density (1-2). Approximately 10-20% of breast cancers are missed by standard mammography – that percentage can approach 40-50% in women with dense breast tissue.
No need to be alarmed. Your breasts are like a majority of US women. Based on the American Journal of Roentology, seventy-four percent of patients between 40 and 49 years old had dense breasts. This percentage decreased to 57% of women in their 50’s. However, 44% of women in their 60’s and 36% of women in their 70’s had dense breasts as characterized on their screening mammograms.
This notification in your report is meant to increase your understanding of your mammogram results. So far, at least 12 states have enacted laws requiring breast imaging centers to add information about breast density in the result notification letters they mail to patients. Legislatures in several other states are considering breast density notification laws, and federal legislation has been proposed.
What Should You Do If You Have Dense Breasts?
If you are found to have dense breasts, the decision on additional screening and about which test—ultrasonography or MRI—should be based on the your lifetime risk of breast cancer.
The American Cancer Society recommends that patients with a lifetime risk of 20% or greater should be screened annually with breast MRI regardless of breast density. This lifetime risk assessment includes those patients who carry the BRCA gene mutations and their untested first-degree relatives.
Also considered are women who underwent chest radiation between the ages of 10 and 30, and patients who have more than one first-degree relative with breast cancer but who do not have an identifiable genetic mutation.
Patients with dense breasts who have an increased lifetime risk but who do not meet these criteria and those who are at average risk may be offered breast ultrasonography. If risk factors are unclear, genetic counseling can help determine the lifetime risk and thus help the patient choose the additional screening test.
MRI, and certain forms of ultrasound, especially automated whole-breast ultrasound, can be very helpful in evaluating women with very dense breast tissue. Mammography and ultrasound together has been shown to be up to 97% sensitive (5).
Kelly et al. demonstrated that supplementing mammography with automated breast ultrasound resulted in doubling the cancer detection rate. The ACRIN 6666 trial showed that supplementing mammography with screening ultrasound in women with an elevated risk of developing breast cancer and dense breast tissue increased the detection rate by 55%.
While WIS does recommend these studies for some patients, realize that there are no formal guidelines by either the American College of Radiology or the American Cancer Society regarding breast imaging for women with dense breast tissue, unless the woman is also considered to be in a high-risk category (for example those with a strong family history of breast cancer).
Some of these tests are not covered by insurance. Also realize that MRI and ultrasound also have some limitations when imaging dense breast tissue – there is no perfect method of evaluation.
Newer methods of mammography such as tomosynthesis and contrast-enhanced mammography are showing promise, but studies are still being performed; these exams may also expose a woman to higher doses of radiation and/or a contrast material injection.
The Bottom Line
Increased breast density makes it harder for a radiologist to detect early stage (read: treatable) breast cancers, which have a tendency to spread faster within dense breasts. If you have dense breasts, know your family history and speak to your primary care doctor about your risk factors and whether an ultrasound or MRI might be helpful in further screening for breast cancer.
Remember, the best way to fight breast cancer is through early screening and detection. WIS recommends:
- Have a mammogram every year starting at age 40 if you are at average risk.
- Have a clinical breast exam at least every three years starting at age 20, and every year starting at age 40.
Further information: The Gail Model calculates a woman’s breast cancer risk over the next five years, in addition to her lifetime risk (www.cancer.gov/bcrisktool/). The model considers age, ethnicity, history of breast cancer in first-degree relatives, age of menarche, and previous history of breast biopsies and benign breast disease. This Risk Assessment Tool can be used by physicians to determine if you are at higher risk for developing breast cancer.
References:
(1) Boyd NF, Guo H, Martin LJ, et al. Mammographic density and the risk and detection of breast cancer. N Engl J Med. 356(3):227-36, 2007.
(2) Tamimi RM, Byrne C, Colditz GA, Hankinson SE. Endogenous hormone levels, mammographic density, and subsequent risk of breast cancer in postmenopausal women. J Natl Cancer Inst. 99(15):1178-87, 2007
(3) Checka CM, Chun JE, Schnabel FR, Lee J, Toth H. The relationship of mammographic density and age: implications for breast cancer screening. AJR Am J Roentgenol. 2012 Mar;198(3):W292-5. doi: 10.2214/AJR.10.6049.
(4) Saslow D, Boetes C, Burke W, et al., American Cancer Society Breast Cancer Advisory Group. American Cancer Society guidelines for breast screening with MRI as an adjunct to mammography. CA Cancer J Clin 2007; 57:75–89.
(5) Kelly KM, Richwald GA. Automated Whole Breast Ultrasound: Advancing the Performance of Breast Cancer Screening. Semin Ultrasound CT MRI 2011; 32:273-280